What is Dercum’s Disease?
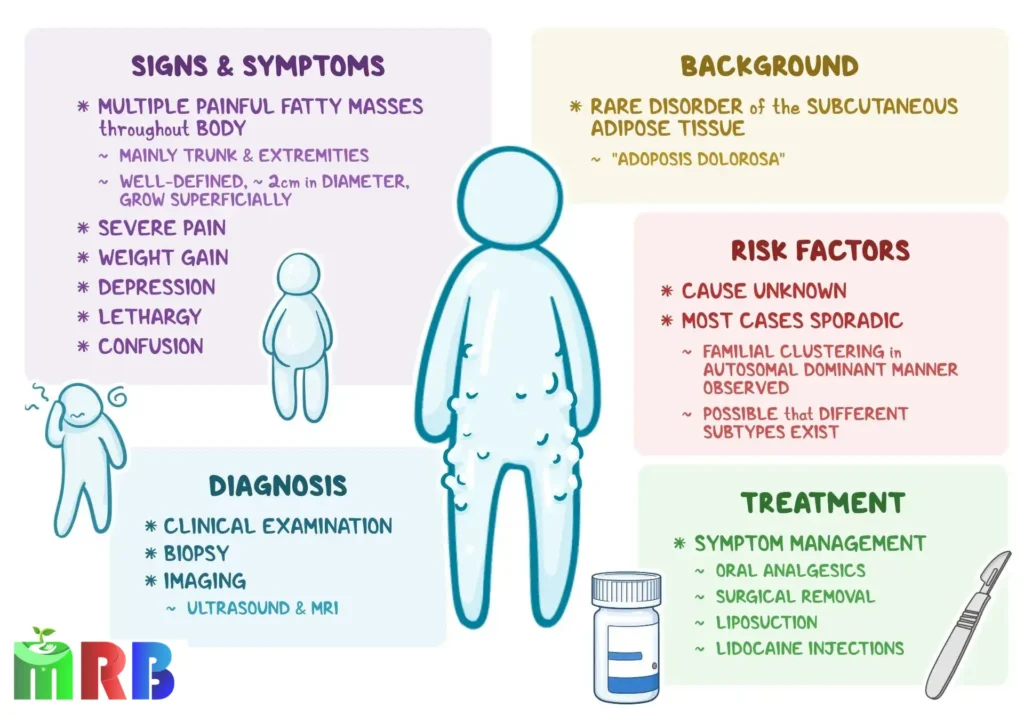
Dercum’s Disease, also known as Adiposis Dolorosa, is a rare and chronic disorder characterized by the development of painful, fatty tumors called lipomas. These lipomas are typically located in subcutaneous tissue, often on the torso, upper arms, upper legs, and buttocks. The condition is more prevalent in women, particularly those who are middle-aged, and is frequently associated with obesity. The pain caused by Dercum’s Disease can range from mild discomfort to severe, debilitating pain, affecting the quality of life for those who suffer from it.
Dercum’s Disease is often misunderstood and misdiagnosed, partly due to its rarity and the lack of widespread awareness. It is classified as a chronic illness because the symptoms tend to persist for a long time, and in many cases, worsen over time.

Symptoms of Dercum’s Disease:
The most prominent symptom of Dercum’s Disease is chronic pain in areas where fatty deposits form. This pain is often described as aching, burning, or stabbing, and it can be persistent or intermittent. Some patients experience localized pain where the lipomas are present, while others feel a more generalized discomfort.
Other common symptoms include:
- Fatigue: Many people with Dercum’s Disease experience chronic fatigue that can severely limit physical activity and reduce energy levels.
- Cognitive Impairment: Known as “brain fog,” patients may have difficulty concentrating, experience memory problems, or feel mentally fatigued.
- Swelling and Fluid Retention: In some cases, the affected areas may swell due to fluid retention, adding to the discomfort.
- Weight Gain: Unexplained weight gain is common, even with a controlled diet and regular exercise. This can be frustrating for patients trying to manage their condition.
- Depression and Anxiety: The chronic pain and physical limitations caused by Dercum’s Disease can lead to emotional challenges, including depression and anxiety.
Causes and Risk Factors
The exact cause of Dercum’s Disease is still not fully understood. However, it is believed to be related to an abnormal growth of fatty tissue combined with an inflammatory response that leads to the painful symptoms. Some theories suggest that it could be linked to hormonal imbalances, immune system dysfunction, or genetic factors. While there is no definitive proof, it is observed that the condition tends to run in families, suggesting a potential hereditary component.
Risk factors for developing Dercum’s Disease include:
- Gender: Women are more frequently diagnosed with Dercum’s Disease than men.
- Age: Most patients are middle-aged, with onset often occurring in the 40s or 50s.
- Obesity: There is a strong correlation between obesity and the development of Dercum’s Disease, though the condition can occur in people of normal weight as well.

Diagnosis
Diagnosing Dercum’s Disease can be challenging due to the rarity of the condition and the overlap of symptoms with other disorders, such as lipedema or fibromyalgia. Physicians typically begin with a thorough medical history and physical examination, focusing on the presence of painful fatty deposits. Imaging studies such as ultrasound, MRI, or CT scans may be used to confirm the presence of lipomas and rule out other potential causes of the pain.
Blood tests may be conducted to exclude other conditions, though there is no specific blood test for Dercum’s Disease. A diagnosis is usually made based on the clinical presentation of the patient and the exclusion of other potential causes.
Treatment Options:
There is currently no cure for Dercum’s Disease, and treatment focuses on managing symptoms. Pain management is a primary concern, and a variety of approaches can be used depending on the severity of the pain and how it affects the individual.
- Medications: Over-the-counter pain relievers, such as NSAIDs, are often ineffective for Dercum’s Disease. Physicians may prescribe stronger pain medications like opioids, although these carry a risk of dependency. Antidepressants and anticonvulsants may also be prescribed to help manage pain and improve mood.
- Liposuction or Surgery: In some cases, the removal of painful lipomas through liposuction or surgery may provide relief. However, the results are often temporary, as lipomas tend to grow back over time.
- Physical Therapy: Some patients find relief through physical therapy, which can help improve mobility and reduce pain. Gentle exercise, such as swimming or walking, can also help improve overall well-being.
- Compression Garments: Wearing compression garments may help reduce pain by providing support to the affected areas and potentially limiting swelling.
- Diet and Weight Management: While weight loss does not cure Dercum’s Disease, maintaining a healthy weight may help reduce symptoms and prevent further worsening of the condition.
Living with Dercum’s Disease
Dercum’s disease can be hard to diagnose and treat. Chronic, severe pain can also lead to problems such as depression and addiction.
If you have Dercum’s disease, consider working with a pain management specialist as well as a mental health professional for added support. You might also find an online or in-person support group for people with rare diseases.
Despite its challenges, it is possible to manage Dercum’s Disease and maintain a good quality of life with the right combination of medical treatment, lifestyle changes, and support.

Do You Have any Query?
Frequently Asked Questiones
Dercum’s Disease, also known as Adiposis Dolorosa, is a rare condition characterized by painful fatty deposits, or lipomas, in the body. These lipomas often form in areas such as the torso, arms, and legs, causing chronic pain and discomfort.
The most common symptoms include:
- Chronic pain in fatty tissue (lipomas)
- Fatigue and lethargy
- Swelling and tenderness in affected areas
- Cognitive difficulties such as “brain fog”
- Weight gain that is difficult to manage
Dercum’s Disease predominantly affects women, particularly those who are middle-aged (40-60 years old). It is often associated with obesity, but it can also occur in people of normal weight. A family history of the disease may increase the risk.
There is no specific test for Dercum’s Disease. Diagnosis is typically made based on a patient’s symptoms, medical history, and the presence of painful lipomas. Imaging techniques like ultrasound or MRI may be used to detect the lipomas, and blood tests may help rule out other conditions.

